As the $1 trillion shift from volume to value is rapidly becoming reality, health systems are responding. The first reality that hits health systems is that the old model of the hospitals as the center of the healthcare universe has led to a catastrophic misalignment of population health resources. Even patients who are heavy utilizers (aka Hot Spotters), spend 99+% of their lives outside the hospital.
The handwriting on the wall couldn’t be clearer for forward-looking health executives: They must develop a sound strategy for addressing that other 99+% of the patient’s life. The old -school, expensive way of accomplishing this objective is to acquire physician practices or post acute care facilities. That approach isn’t working very well with record levels of burnout and even suicide amongst doctors and little improvement in outcomes or cost reductions that will be the difference between winning and losing in the "no outcome, no income" era. It’s common sense that winning health systems will put a focus on the Quadruple Aim as an alternative. Fortunately, there are leaders such as Dr. Kenneth Adams, VP of Post Acute Care at Texas Health Resources (THR), who realize there is a smarter way to approach care after a patient leaves the hospital.
Virtual Integrated Health Network focuses on $1 billion spent after hospitalizations
When I spoke with Adams, he shared that they send 3,000 to 4,000 patients per month to post acute settings such as skilled nursing facilities, rehabilitation centers or to the patient’s home with the help of home care resources. In the flawed, old reimbursement model, it was out of sight, out of mind. With the perverse incentives of old, a hospital was actually rewarded when someone came back with an avoidable readmission. Slowly, but surely, healthcare purchasers are wising up to the fact that the vast majority of hospitalizations represent an abject failure of the health system to catch something earlier or prevent it entirely.
THR estimates that spending in the post acute settings is approximately $1 billion. Whether THR is under a captitated model or trying to avoid hospitalization readmission penalties, they have mobilized to create a Virtual Integrated Health Network (vIDN). For a time, THR strongly considered going the old school route of gobbling up organizations as many have done. They wisely recognized the value of care delivery using the existing post-acute labor force enabled through inexpensive cloud solutions. This made more sense as a way to create a high value network they could trust would care for patients properly. They were also mindful that Dallas has had two of the largest home health frauds in the country, so having transparency into what was happening after a hospitalization was critical.
The problem is that legacy EMRs, quite logically, are optimized to generate as much fee-for-service revenue as possible. It's no small challenge for health systems to shift from thinking of a hospitalization as a "success" to recognizing it is a failure in most instances. Naturally, the way legacy EMR systems such as Epic were implemented was to customize in a way that reflected the pre-Copernican view of healthcare where the hospital was at the center of the healthcare universe. Implicitly it treated hospitalizations as "success" when the vast majority could have been avoided with a proper focus on optimizing health, not revenues. While systems such as Epic are quite customizable when they are originally set up, they are notoriously rigid once the setup phase is completed. In the post-Copernican view of healthcare that THR is focused on, they recognized they needed a different solution that reflects the importance of understanding the full picture of what’s going on with a patient — not just what was going on at the hospital.
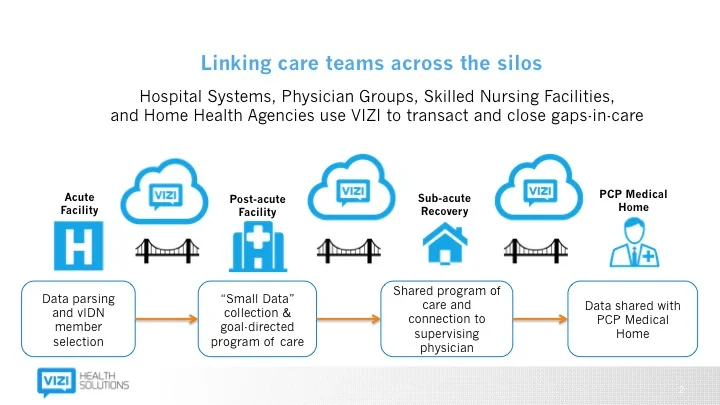
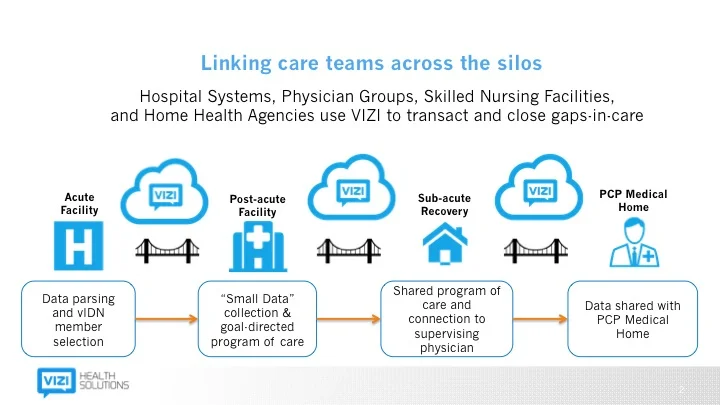
The schematic below represents the way forward-looking, post-Copernican health system leaders are viewing how they organize their population health efforts (click the image to get the detailed view).
After coming to the conclusion that THR needed to create what some would call a “narrow network” of high quality post acute providers, it was clear that their Epic system wasn’t built with that in mind. With clarity on their vision and requirements, they sought out a solution and found VIZI Health Solutions. VIZI is an important tool to create a new standard of care whether someone is inside or outside of THR.
In the Dallas/Fort Worth area, there are 300 skilled nursing facilities (SNFs), as an example. The quality varies widely so THR is focused on working with the highest quality organizations. Just as the EMRs inside the hospitals were logically optimized for billing, so too are the EMRs inside of SNFs. Thus, VIZI’s solution is critical to providing the SNFs new capabilities. After the excruciating process of implementing their EMR, there was surprise at how quickly they were able to stand up each clinic (under a week).
In the old model, a SNF might receive a fax with information on a patient. It was usually incomplete. The result was sub-optimal care as the individual arrives as virtually a newborn in terms of knowledge of the patient's medical history. Of course, nurses and doctors do their best work when they have a more complete view of a patient. That’s what VIZI provides. They replace the fax to dramatically improve the care transition. For the SNF, simply knowing in advance what medications a patient is taking can help them save a considerable amount — something that is particularly important if they are receiving a fixed payment to deliver care.
Small Data: A New Solution for a Big Healthcare Problem
While we’re in the full hype phase of Big Data, Adams recognized that "Small Data” would give THR a unified assessment that draws on non-clinical impacts. Historically, Adams said that doctors tend to focus on vital signs. However, it won’t show up in a typical EMR assessment if someone hasn’t been able to get out of bed. VIZI starts looking at those things. Medical data isn’t always the most important item. For example, is there food in fridge or is A/C working — these things are more predictive of a hospitalization than most vital signs.
Dr. Mark Ridinger is the Chief Medical Information Officer of VIZI Health Solutions who has helped architect VIZI’s solution to address these scenarios as he explained in a recent blog post.
As we start to pay more attention to the needs of our complex elder patients after hospital discharge, health systems are realizing that they can’t mitigate risk and improve outcomes with broken data links which occur after the patient leaves the hospital setting and transitions home. Small data is going to offer solutions to some pretty big challenges posed by the shift to outcomes-based reimbursement models, and as we collectively redefine what it means to be healthy in a more holistic context. This new focus on transitional care is all about small—not big—data.
Big data has been defined as encompassing the four V’s: volume, velocity, variety, and veracity of information. We see small data in the healthcare setting as encompassing “four P’s”: punctual, purposeful, prognostic, and at the point-of-living.
THR chose a logical area to focus their early efforts -- total joint replacements. As I reported earlier, bundled payments are here to stay. Just up the road, they can see that the logical next step after bundled payments is true price transparency. The largest non-profit health system in the country is using transparent pricing to gain a market advantage over their competitors via a Transparent Medical Network. In a future piece, I'll report on a related development beyond bundled, transparent pricing -- warrantying procedures. Organizations confident in their costs and quality recognize this is another way to not only deliver the best possible value but also gain a market advantage. In the past, healthcare purchasers have rewarded mediocrity. Paradoxically, I reported last week on how the best way to slash healthcare costs is to improve health benefits. For example, with superior benefits a medium-sized employer is saving 50% per capita on health benefits while a small employer is saving 30% per capita by implementing portions of the Health Rosetta healthcare purchasing blueprint. Since these steps are so straightforward, one could argue that CEOs and CFOs are failing in their fiduciary responsibility to not implement components of the Health Rosetta. THR is positioning themselves for that day.
[Disclosure: As I've disclosed many times, the Health Rosetta is a non-commercial open-source project that provides a reference model for how purchasers of healthcare should procure health services. In my role as managing partner of Healthfundr, a seed stage venture fund, the Health Rosetta is the foundation of our investment thesis.]
Clear ROI for Health System and Post Acute Facility
Smart post acute providers are embracing the vIDN approach. Their old model of marketing to discharge coordinators at a hospital is unscientific,unproductive, and costly.. They would much rather have an integrated model that allows them to deliver better care at a lower price (e.g., using generic alternatives that are equally effective to expensive branded drugs). Post acute providers also realize that if they aren’t a part of the vIDN, they stand to lose a lot of patient volume.
A couple admissions a month easily pays for the license fee. Thus, the ROI for the post acute facility is a no-brainer. Cinching the deal for the health system that pushes for the adoption of the vIDN is that they aren’t saddled with an epic license fee. Rather, smart post acute facilities are more than happy to pay for the license fees to participate in the vIDN. It's free for the health system organizing the vIDN.
Adams indicated that he was fortunate to have a visionary boss who wants to do what is best for patients. It would take the most pessimistic and narrow-minded executive to not recognize that this will be a great business model for delivering outstanding care even if every step of that journey isn’t crystal clear. Most health systems benefit from having a good size war chest to learn and evolve their model during the transition. THR looks like they are avoiding the newspaper industry approach that many health systems are guilty of today. To their credit, THR is more the exception than the rule. Most health system executives I speak with are acting remarkably similar to newspaper executives in the late 90s and early 2000s. THR is determined to avoid that fate. Quite the contrary, with $1 trillion of annual revenue shifting to new players and business models over the coming decade, there will be huge winners and huge losers. With the vIDN move, THR is positioning itself to be one of the winners.
Subscribe to The Future Health Ecosystem Today or follow on Twitter
Contact via Healthfundr for expertise requests or speaking engagements
Upcoming travel/speaking schedule present opportunities to get on Dave's speaking calendar:
- Week of March 28: Washington DC
- Week of April 4: Montreal, Chicago
- Week of April 25: Orlando
- Week of June 13: New York City
- Week of July 4: Toronto
- Week of July 25: Montana
- Week of September 19: Northern Europe